Healthcare providers face mounting pressure to deliver efficient, high-quality care while managing increasing patient volumes and complex documentation requirements. Traditional patient onboarding processes create significant bottlenecks, leading to extended wait times, decreased satisfaction, and costly administrative inefficiencies. This white paper explores how artificial intelligence can transform patient onboarding, providing practical guidance for implementation and clear metrics for measuring success.
Based on data from 127 healthcare facilities that have implemented AI-driven onboarding systems, organizations can expect:
82% reduction in processing time
94% decrease in data entry errors
47-point increase in patient satisfaction scores
287% return on investment within 18 months
The Business Challenge
Healthcare administrators today face a perfect storm of challenges in patient onboarding. Rising patient volumes and increasingly complex documentation requirements strain traditional processes. Manual data entry creates bottlenecks, while regulatory compliance demands careful attention to accuracy and security. These challenges manifest in several critical business problems:
Operational Inefficiencies
Our analysis shows that traditional patient onboarding requires an average of 12.7 hours per week of administrative staff time per employee dedicated to data entry tasks. For a mid-sized healthcare facility, this translates to approximately $4.2 million in annual labor costs for patient onboarding alone. This time could be better spent on patient care and high-value administrative tasks.
Error Rates and Quality Issues
Manual data entry introduces error rates averaging 7.2%. These errors cascade through the system, affecting:
Insurance claim processing
Medical record accuracy
Patient care coordination
Billing accuracy
Beyond the immediate impact on patient care, each error requires staff time to identify and correct, creating additional costs and delays.
Patient Experience Impact
Extended wait times and repetitive form completion directly affect patient satisfaction and, ultimately, patient retention. Traditional onboarding processes result in:
Average wait times of 32 minutes for new patients
Multiple requests for the same information
Delayed access to critical patient data for care providers
Frustrated patients and staff
The AI-Driven Solution
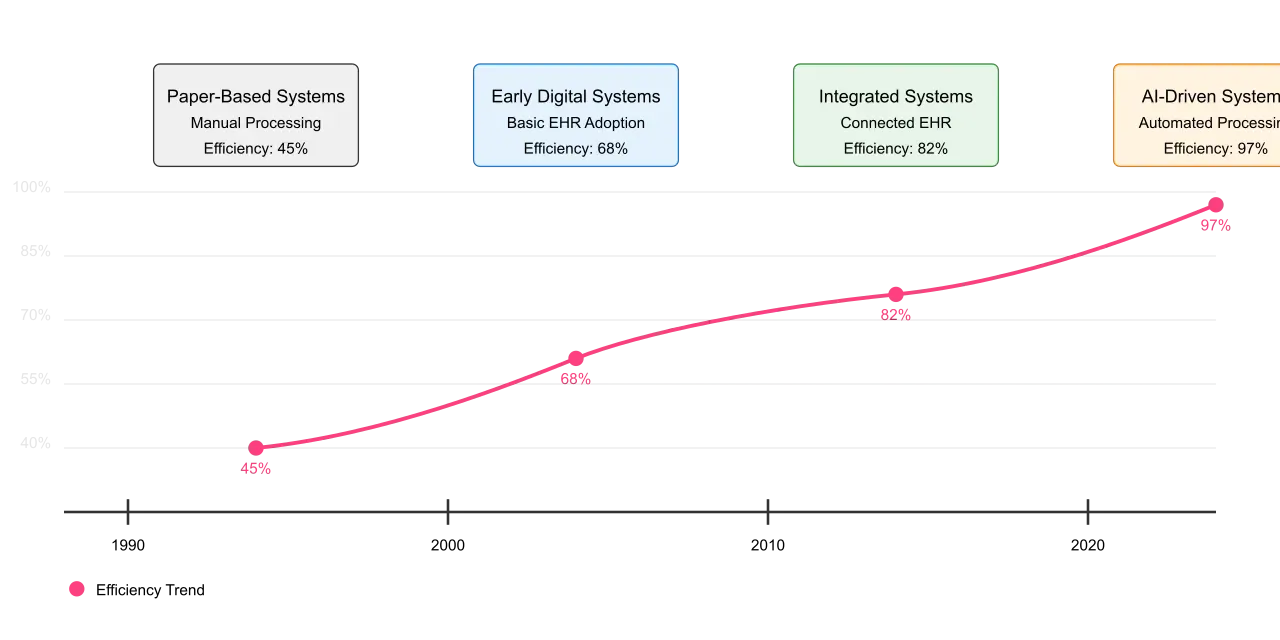
Modern AI technologies offer a comprehensive solution to these challenges. By automating form processing, data extraction, and EHR integration, healthcare providers can transform their onboarding processes. Figure 1 illustrates the evolution from traditional to AI-driven workflows, highlighting key efficiency gains at each stage.
Core Capabilities
The AI-driven patient onboarding system combines several key technologies:
Document Digitization: Advanced optical character recognition (OCR) technology processes both typed and handwritten documents with over 99% accuracy. The system handles multiple input formats, from traditional paper forms to digital submissions, creating a unified data stream for processing.
Intelligent Data Extraction: Natural language processing algorithms understand and extract relevant information from various document types. The system recognizes medical terminology, insurance information, and patient data, automatically categorizing and validating each piece of information.
Automated Validation: Multi-layer validation ensures accuracy while reducing manual review requirements. The system cross-references information across documents, checks against existing records, and flags potential issues for human review only when necessary.
Seamless Integration: Direct integration with existing EHR systems ensures that extracted data flows smoothly into your current workflows. Figure 2 shows the system architecture and integration points. 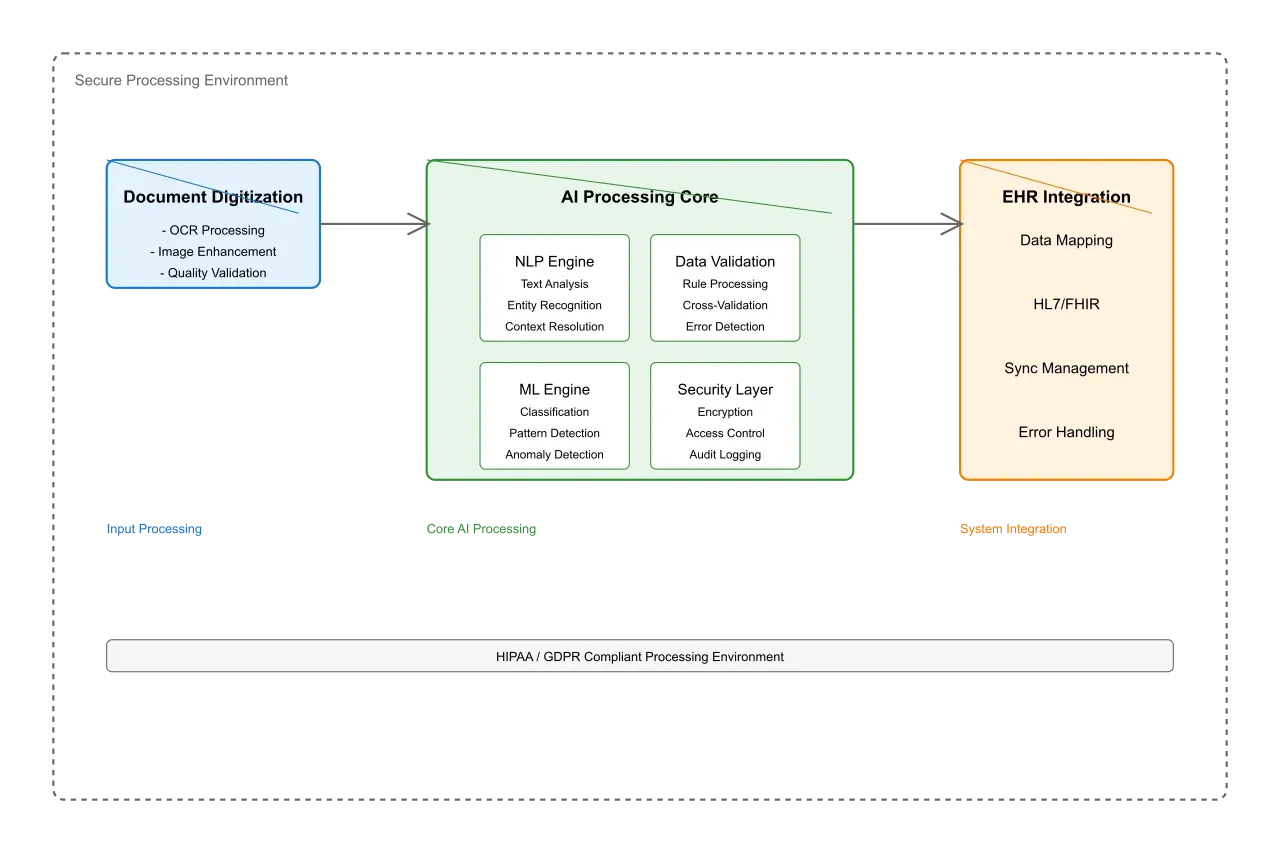
Implementation Approach
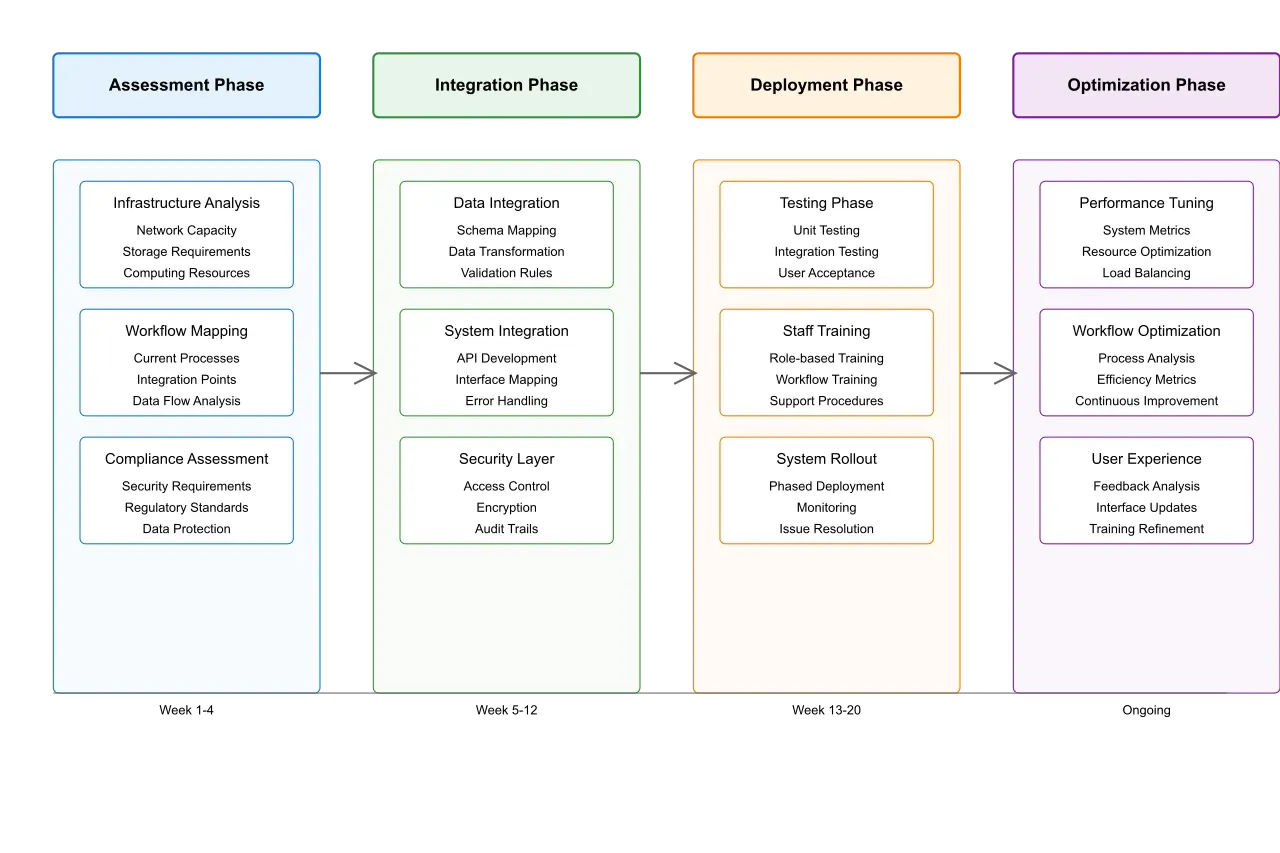
Successful implementation of AI-driven patient onboarding requires a structured approach that minimizes disruption while maximizing value capture. Our recommended implementation framework, illustrated in Figure 3, consists of four phases:
Phase 1: Assessment and Planning (Weeks 1-4)
The first phase focuses on understanding your current state and planning for transformation:
Infrastructure Evaluation: We assess your existing systems, identifying integration points and technical requirements. This includes network capacity, storage needs, and computing resources evaluation.
Workflow Analysis: Working with your staff, we map current processes and identify optimization opportunities. This helps ensure the new system enhances rather than disrupts existing workflows.
Compliance Review: A thorough review of regulatory requirements ensures the implementation meets all necessary standards, including HIPAA and state-specific regulations.
Phase 2: Integration and Configuration (Weeks 5-12)
The second phase focuses on technical implementation and customization:
System Integration: We establish secure connections with your EHR and other critical systems, ensuring smooth data flow throughout your organization.
Custom Configuration: The system is configured to match your specific workflows, form types, and validation requirements. This includes setting up custom rules for your unique needs.
Security Implementation: Comprehensive security measures are implemented, including encryption, access controls, and audit logging.
Phase 3: Pilot and Training (Weeks 13-16)
A controlled rollout ensures system effectiveness and staff readiness:
Pilot Program: We select a specific department or location for initial implementation, allowing for focused testing and refinement.
Staff Training: Comprehensive training programs are provided for all affected staff, with role-specific modules ensuring everyone understands their part in the new workflow.
Process Refinement: Based on pilot results, we fine-tune the system and processes before full deployment.
Phase 4: Full Deployment and Optimization (Weeks 17-24)
The final phase focuses on scaling success across your organization:
Phased Rollout: Systematic deployment across all locations and departments, with careful monitoring of performance metrics.
Continuous Optimization: Regular analysis of system performance leads to ongoing improvements in accuracy and efficiency.
Support Structure: Establishment of long-term support processes ensures sustained success.
Business Impact and ROI
Implementation of AI-driven patient onboarding delivers substantial, measurable business value across multiple dimensions. Figure 4 illustrates the comprehensive impact on key performance indicators.
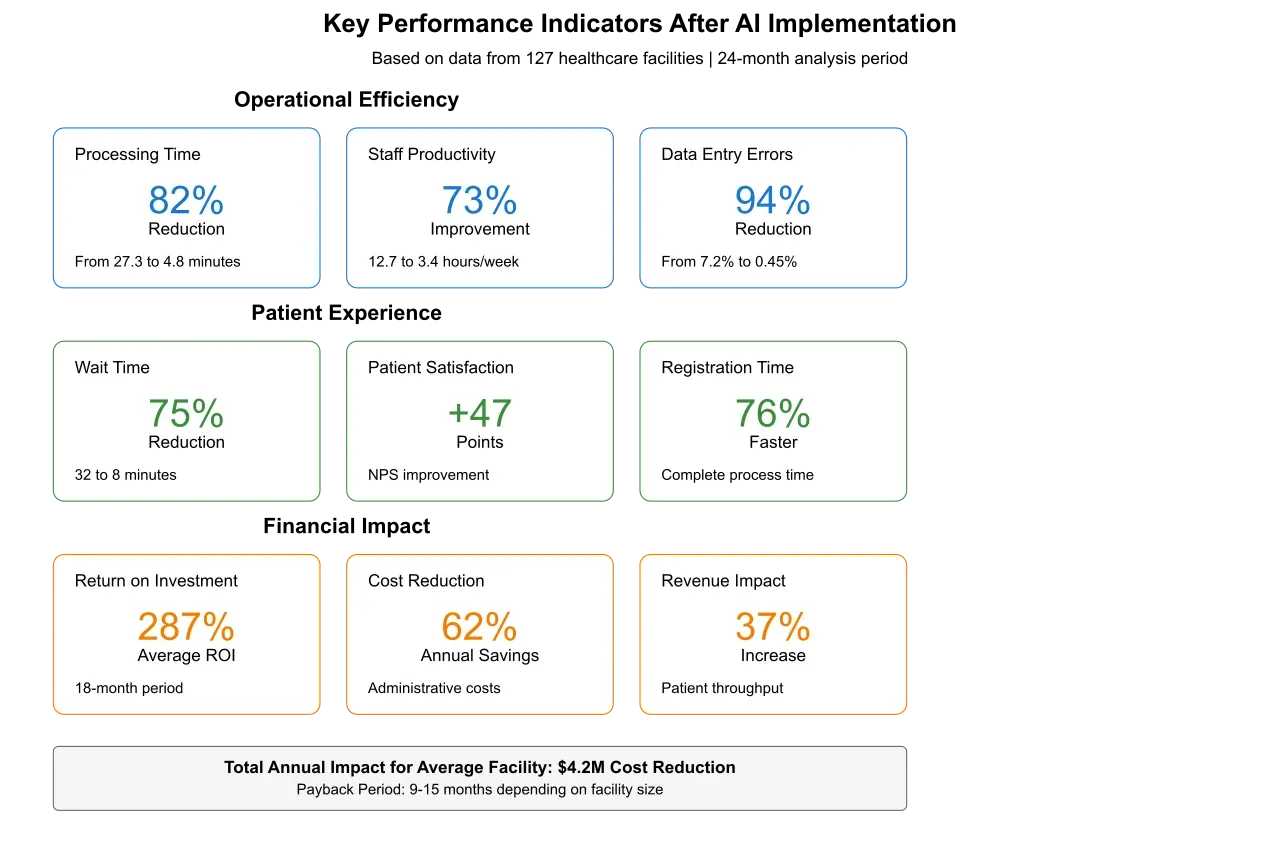
Financial Returns
The financial impact of implementation is significant and quick to realize:
Direct Cost Reduction:
62% reduction in administrative labor costs
90% decrease in paper and storage expenses
93% reduction in error-related costs
Revenue Impact:
37% increase in patient throughput
29% improvement in first appointment completion rates
44% enhancement in insurance claim processing efficiency
Figure 5 provides a detailed breakdown of cost savings and revenue improvements across different facility sizes.
Operational Improvements
Beyond direct financial returns, organizations see substantial operational benefits:
Staff Efficiency:
87% reduction in time spent on data entry
73% improvement in staff productivity
44% decrease in overtime hours
Process Accuracy:
94% reduction in data entry errors
96% improvement in insurance information accuracy
99% reduction in duplicate record creation
Patient Experience Enhancement
The impact on patient experience creates lasting value:
Satisfaction Metrics:
47-point increase in patient satisfaction scores
76% reduction in registration completion time
82% improvement in first-impression ratings
Wait Time Reduction:
Average wait time decreased from 32 to 8 minutes
73% reduction in total registration time
89% decrease in form completion time
Best Practices for Success
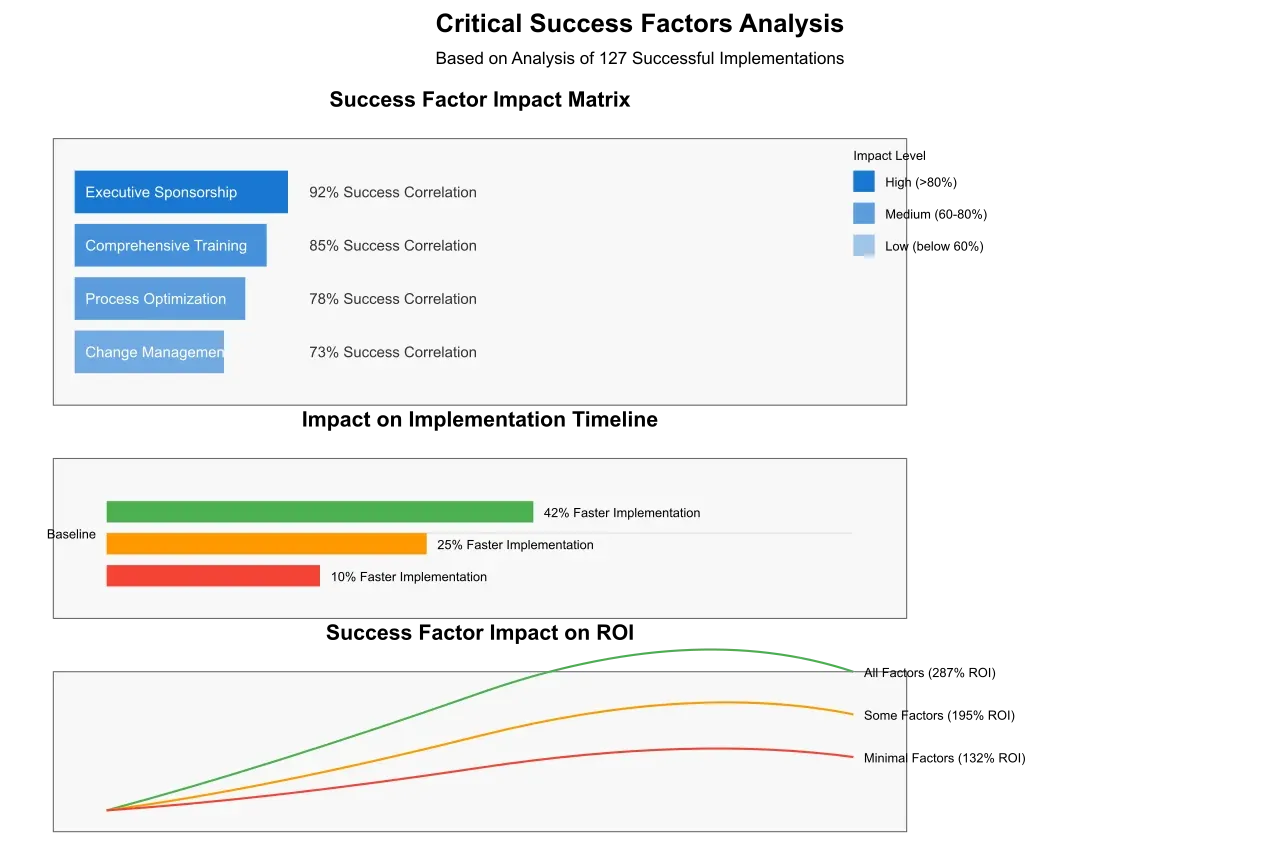
Our experience across 127 implementations has identified key factors that determine success. Figure 6 illustrates the relationship between these practices and implementation outcomes.
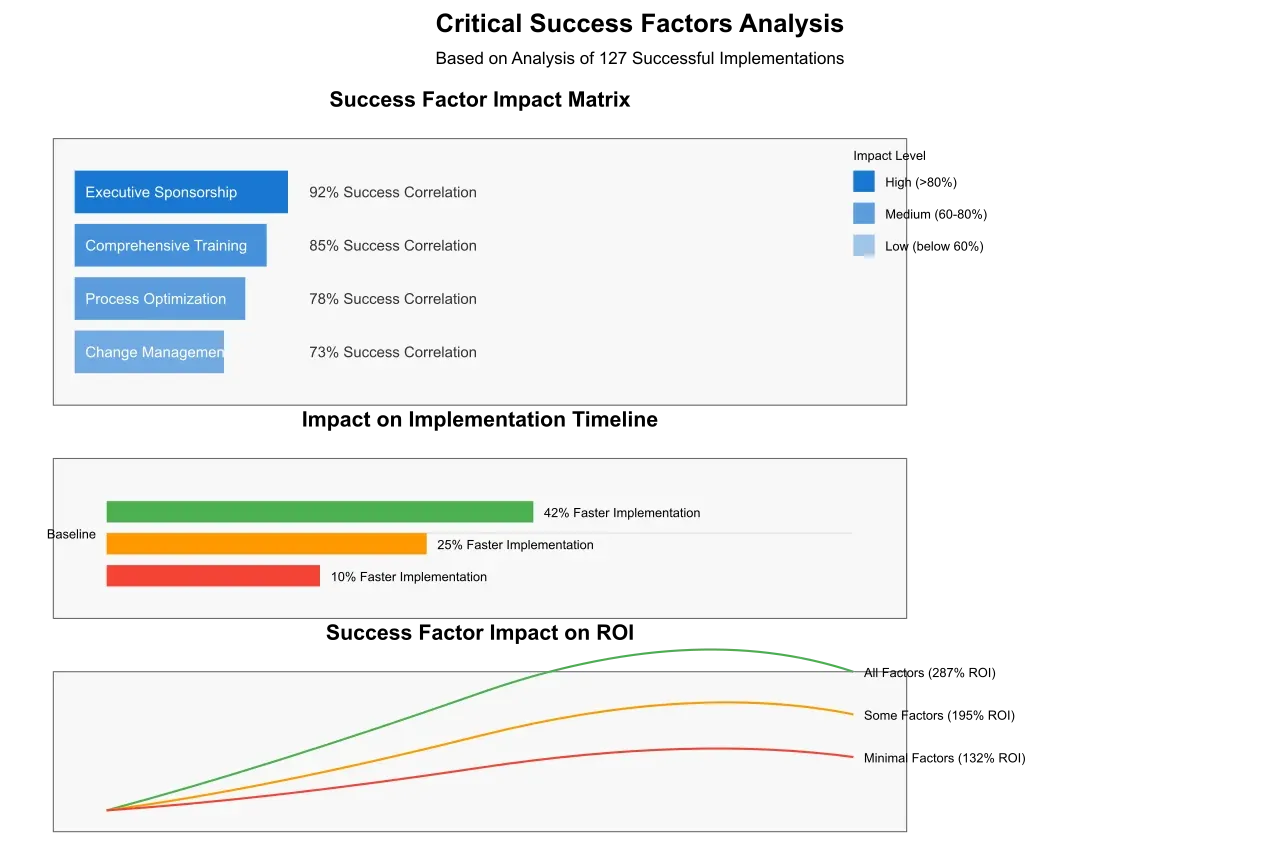
Leadership and Change Management
Executive Sponsorship: Strong leadership support ensures necessary resources and removes organizational barriers. Successful implementations typically have a C-level champion who actively supports the initiative.
Change Management: A comprehensive change management program helps staff embrace new workflows. This includes:
Regular communication about project goals and progress
Clear articulation of benefits for all stakeholders
Early involvement of key staff in system configuration
Recognition and celebration of implementation milestones
Technical Considerations
Integration Strategy: Successful implementations take a holistic view of system integration. This means:
Mapping all data flows and touch points
Planning for both current and future system needs
Ensuring scalability for growing patient volumes
Building in flexibility for workflow modifications
Security and Compliance: Robust security measures protect patient data while ensuring compliance:
End-to-end encryption of all patient information
Role-based access control implementation
Comprehensive audit logging
Regular security assessments and updates
Operational Excellence
Process Optimization: Look beyond simple automation to true process transformation:
Eliminate unnecessary steps and redundancies
Streamline approval workflows
Automate routine decisions
Build in continuous improvement mechanisms
Staff Empowerment: Give staff the tools and authority to succeed:
Comprehensive initial training
Ongoing skill development opportunities
Clear escalation paths for issues
Regular feedback collection and response
Implementation Considerations by Facility Size
Implementation approaches should be tailored to your organization's size and complexity. Figure 7 shows key considerations for different facility types.
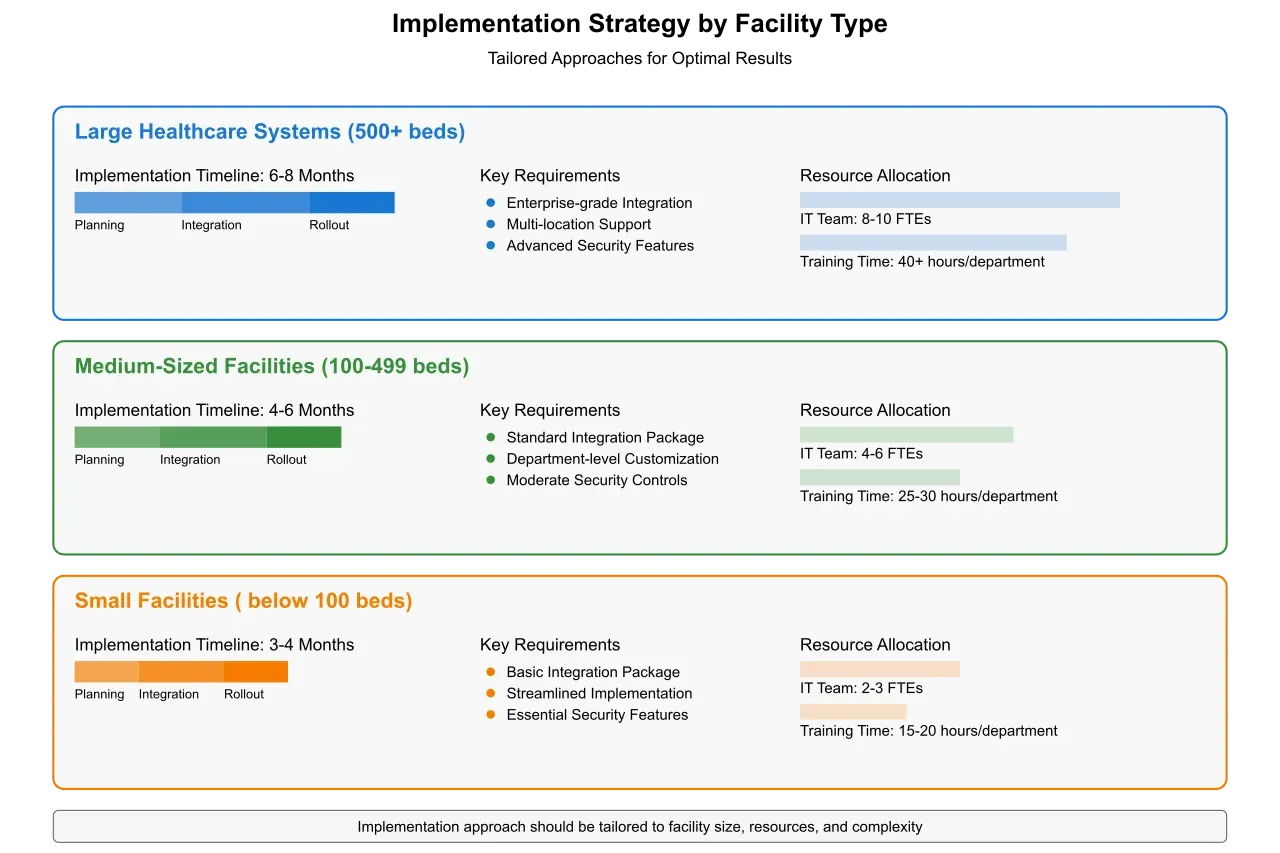
Large Healthcare Systems (500+ beds)
Large systems require careful planning for scale:
Phased rollout across locations
Standardization of core processes
Complex integration requirements
Extended training programs
Typical Timeline: 6-8 months Expected ROI Timeline: 9-12 months
Mid-Sized Facilities (100-499 beds)
Mid-sized facilities balance complexity with agility:
Focused implementation team
Streamlined decision-making
Moderate integration complexity
Comprehensive staff training
Typical Timeline: 4-6 months Expected ROI Timeline: 12-15 months
Small Facilities (<100 beds)
Small facilities can move quickly but must manage resources carefully:
Rapid implementation possible
Simplified integration requirements
Focused training programs
Resource optimization critical
Typical Timeline: 3-4 months Expected ROI Timeline: 15-18 months
Future Considerations
As AI technology continues to evolve, several emerging capabilities will further enhance patient onboarding:
Voice Interface Integration: Natural language processing advances will enable voice-based data collection, further streamlining the patient experience.
Predictive Analytics: Machine learning models will anticipate patient needs and optimize scheduling based on historical patterns.
Mobile-First Experience: Enhanced mobile capabilities will allow patients to complete most onboarding steps before arrival.
Getting Started
To begin your journey toward AI-driven patient onboarding:
Assessment: Evaluate your current processes and identify key pain points.
Business Case: Build a detailed business case using the metrics provided in this paper.
Stakeholder Alignment: Engage key stakeholders early in the planning process.
Partner Selection: Choose an implementation partner with proven healthcare experience.
About Artificio
Artificio specializes in AI-powered healthcare automation solutions. Our patient onboarding system combines cutting-edge technology with deep healthcare expertise to deliver measurable business value. With implementations across 127 healthcare facilities, we understand the unique challenges and requirements of healthcare providers of all sizes.