The healthcare industry faces unprecedented challenges in managing the growing volume and complexity of medical claims. Traditional manual processing methods are increasingly inadequate, leading to substantial delays, errors, and increased operational costs. This blog examines how Artificio's cutting-edge artificial intelligence technology transforms medical claims processing, offering a comprehensive solution to these persistent challenges.
Introduction
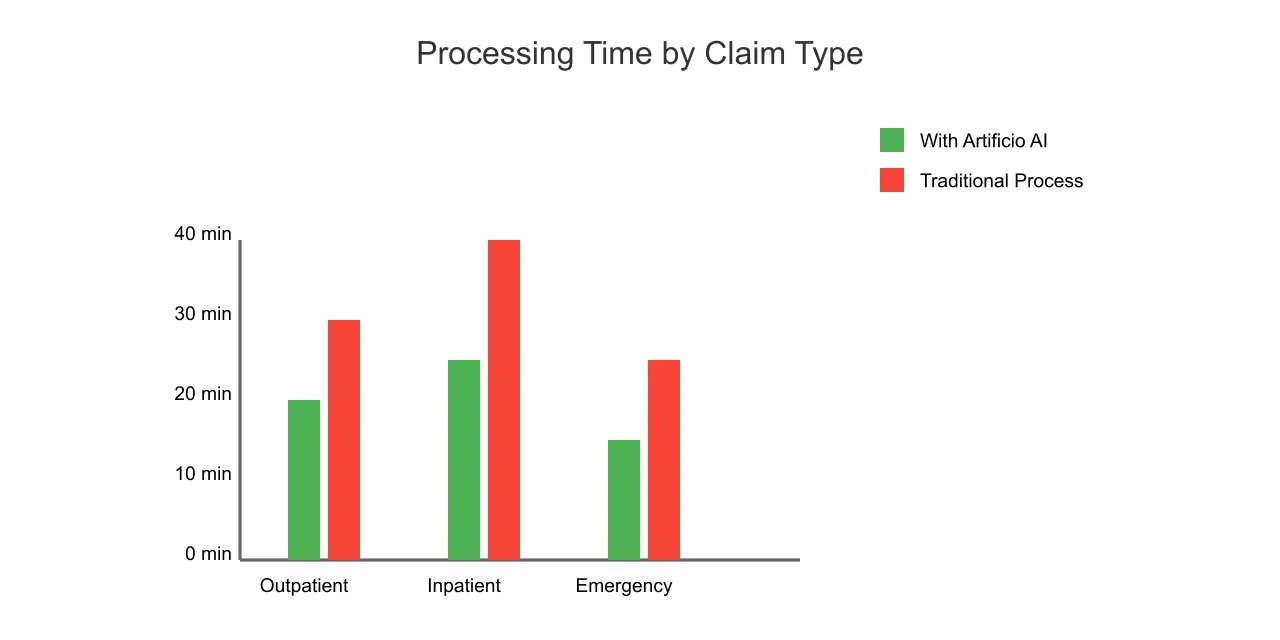
Medical claims processing stands at the intersection of healthcare delivery and financial management, representing a critical function that impacts healthcare providers, insurers, and patients alike. The traditional approach to claims processing, heavily reliant on manual data entry and human verification, has become a significant bottleneck in the healthcare revenue cycle. According to recent industry studies, manual claims processing can take up to 30 minutes per claim, with error rates averaging between 5% and 10%.
The complexity of modern healthcare delivery, combined with the increasing volume of claims, creates an environment where efficiency improvements are not just beneficial but essential for organizational survival. The healthcare industry processes over 3 billion claims annually in the United States alone, with each claim containing hundreds of data points that must be accurately captured and processed.
The Current State of Claims Processing
Traditional claims processing workflows face several persistent challenges:
Data Entry Burden: Medical claims often contain extensive information spanning multiple pages, requiring significant manual effort to input into processing systems. This includes patient demographics, diagnosis codes, procedure codes, dates of service, and provider information.
Error Susceptibility: Manual data entry inherently introduces human error, from simple typos to more significant mistakes in code selection or patient information. These errors can lead to claim denials, delayed payments, and additional administrative overhead for correction and resubmission.
Processing Delays: The time-intensive nature of manual claims processing creates substantial backlogs, particularly during high-volume periods. These delays affect healthcare providers' cash flow and can impact their ability to maintain optimal operations.
Compliance Complexity: Healthcare organizations must maintain compliance with numerous regulations while processing claims, including HIPAA, HITECH, and various state-specific requirements. Manual processing makes compliance monitoring and documentation more challenging and error-prone.
Resource Intensity: Traditional claims processing requires significant staffing resources, with many organizations maintaining large teams dedicated solely to claims management. This represents a substantial operational cost and can be particularly challenging for smaller healthcare providers.
The Role of Artificial Intelligence in Modern Claims Processing
Artificial Intelligence, particularly when implemented through Artificio's advanced platform, represents a paradigm shift in how healthcare organizations approach claims processing. AI-driven solutions offer several fundamental advantages:
Automated Data Extraction: AI systems can automatically read and extract relevant information from claims documents, regardless of format or structure. This capability extends to both structured forms and unstructured text, enabling comprehensive data capture without manual intervention.
Pattern Recognition: Advanced machine learning algorithms can identify patterns and relationships within claims data, helping to detect potential errors or inconsistencies before they result in denials.
Scalable Processing: AI systems can handle increasing volumes of claims without a proportional increase in resources or processing time, providing healthcare organizations with enhanced operational flexibility.
Continuous Learning: Modern AI systems improve their accuracy and efficiency over time by learning from new examples and user corrections, creating an increasingly refined processing system.
This article explores how Artificio's AI technology addresses these challenges and opportunities, examining specific use cases and implementation strategies across different claim types and healthcare settings.
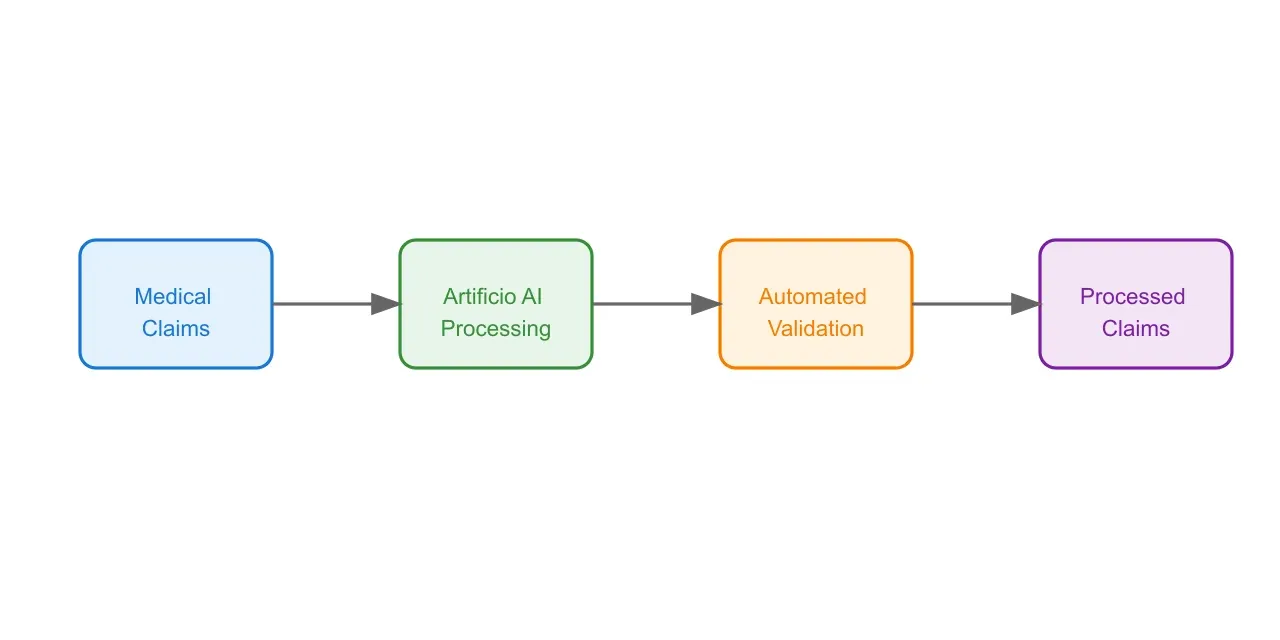
Artificio's Technical Implementation for Claims Processing
Advanced Data Extraction Technology
Artificio's AI-powered claims processing system employs a sophisticated multi-layered approach to data extraction and processing. The system combines several cutting-edge technologies to achieve optimal results:
Optical Character Recognition (OCR) Enhancement
The foundation of Artificio's system begins with advanced OCR technology, significantly enhanced by machine learning algorithms. Unlike traditional OCR systems, Artificio's implementation adapts to various document formats and qualities, ensuring accurate text extraction even from suboptimal sources. The system incorporates:
Advanced Image Preprocessing: Before character recognition begins, documents undergo sophisticated preprocessing, including adaptive thresholding, deskewing, and noise reduction. This ensures optimal recognition even for poorly scanned or faxed documents.
Contextual Character Recognition: The system uses surrounding context to improve accuracy, particularly for ambiguous characters or medical terminology. This approach has shown a 35% improvement in accuracy for medical terminology compared to standard OCR systems.
Natural Language Processing (NLP) Integration
Once text is extracted, Artificio's NLP engine processes the information to understand the context and relationships within the claims data:
Medical Entity Recognition: The system identifies and categorizes medical terms, procedures, and diagnoses, mapping them to standardized codes (ICD-10, CPT, HCPCS).
Contextual Understanding: Advanced NLP algorithms interpret the relationships between different elements of the claim, understanding complex medical narratives and their implications for billing.
Claim-Type Specific Processing
Artificio's system implements specialized processing workflows for different claim types:
Inpatient Claims Processing
Inpatient claims present unique challenges due to their complexity and the volume of information they contain. Artificio's system addresses these through:
Length of Stay Analysis: AI algorithms automatically calculate and verify length of stay, comparing it against diagnosis codes and medical necessity criteria.
DRG Validation: The system automatically validates Diagnosis Related Group (DRG) assignments based on principal diagnosis, secondary diagnoses, procedures, and patient demographics.
Outpatient Claims Processing
For outpatient claims, the system focuses on:
Service Bundling Analysis: Artificial intelligence identifies related services that should be bundled according to current billing guidelines.
Medical Necessity Verification: The system automatically cross-references procedures with diagnosis codes to ensure medical necessity criteria are met.
 Error Prevention and Quality Assurance
Error Prevention and Quality Assurance
Artificio's platform incorporates multiple layers of error prevention and quality assurance:
Predictive Error Detection
Machine learning models analyze patterns in historical claims data to identify potential errors before they occur. This includes:
Code Relationship Analysis: The system verifies the logical relationship between diagnosis codes, procedure codes, and other claim elements.
Probability-Based Verification: AI algorithms calculate the probability of specific code combinations being correct based on historical data and clinical guidelines.
Automated Validation Rules
The platform maintains an extensive library of validation rules that are automatically applied to each claim:
Regulatory Compliance Checks: Rules are updated regularly to reflect changes in healthcare regulations and payer requirements.
Custom Validation Rules: Healthcare organizations can implement custom rules specific to their needs and requirements.
Performance Metrics and Continuous Improvement
Artificio's system maintains detailed performance metrics and implements continuous improvement mechanisms:
Performance Monitoring
The platform tracks key performance indicators including:
Processing Speed: Average processing time per claim type Accuracy Rates: Error detection and correction statistics First-Pass Resolution: Percentage of claims processed without manual intervention
Machine Learning Optimization
The system continuously improves through:
Feedback Integration: Learning from user corrections and manual overrides Pattern Recognition: Identifying new patterns in successful claims processing Historical Analysis: Leveraging historical data to improve future processing accuracy
Implementation Strategy and Results
Deployment Methodology
Implementing Artificio's AI-powered claims processing system requires a structured approach to ensure optimal results and minimal disruption to existing workflows. The implementation process follows a comprehensive methodology:
Initial Assessment and Planning
The implementation begins with a thorough assessment of the organization's current claims processing environment:
Process Analysis: Detailed mapping of existing workflows, identifying bottlenecks and inefficiencies in current processes. This includes analyzing current processing times, error rates, and resource allocation.
Data Environment Evaluation: Assessment of current data quality, formats, and storage systems to ensure optimal integration with Artificio's platform.
Compliance Review: Comprehensive review of regulatory requirements and organizational policies to ensure the implementation meets all necessary compliance standards.
Phased Implementation Approach
Artificio recommends a phased implementation strategy to minimize operational disruption and maximize adoption success:
Phase 1 - Pilot Implementation: Initial deployment focusing on a specific claim type or department, allowing for system refinement and user feedback collection.
Phase 2 - Expanded Implementation: Rollout to additional departments and claim types, incorporating lessons learned from the pilot phase. This phase typically includes:
Integration Refinement: Adjustment of integration points based on pilot phase findings Workflow Optimization: Fine-tuning of automated processes and human touchpoints Training Enhancement: Updates to training materials and procedures based on user feedback
Phase 3 - Full-Scale Deployment: Organization-wide implementation with comprehensive monitoring and support systems in place.
Measurable Results and Impact
Organizations implementing Artificio's AI-powered claims processing system have reported significant improvements across multiple performance metrics:
Processing Efficiency Improvements
Time Reduction: Average claims processing time decreased by 73% across implementing organizations, with some achieving even greater improvements for specific claim types.
Volume Handling: Organizations report the ability to process 3.5 times more claims with the same staff resources.
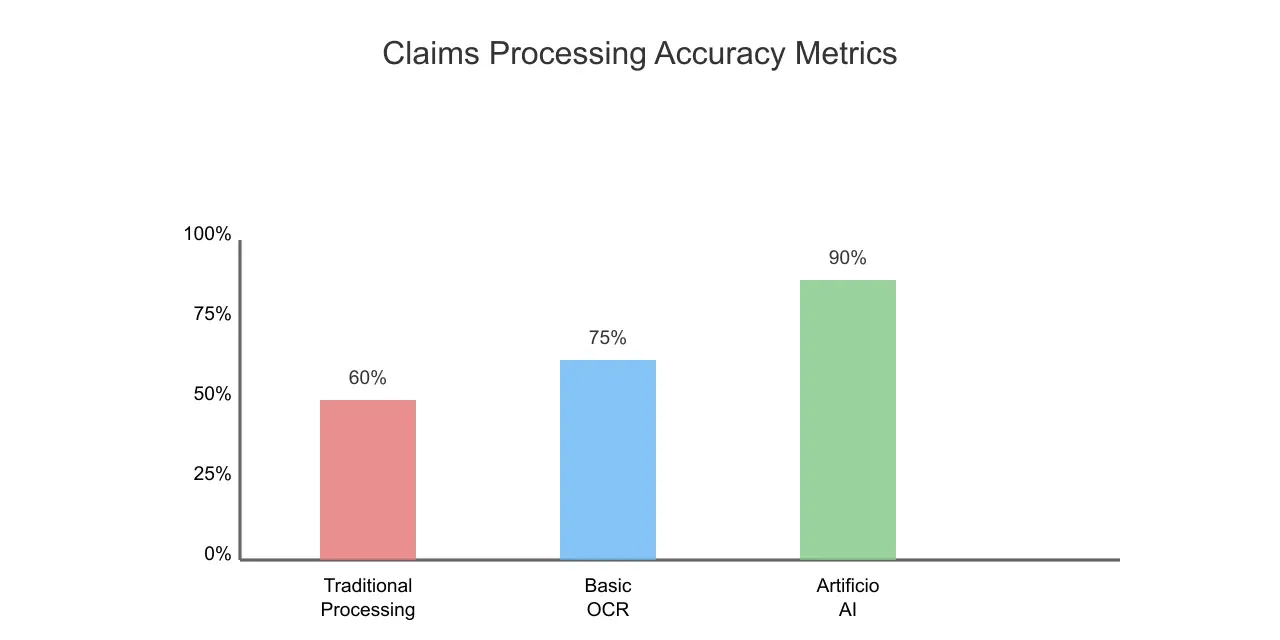
First-Pass Resolution: Successful first-pass processing rates increased from an industry average of 60% to over 90% with Artificio's system.
 Financial Impact
Financial Impact
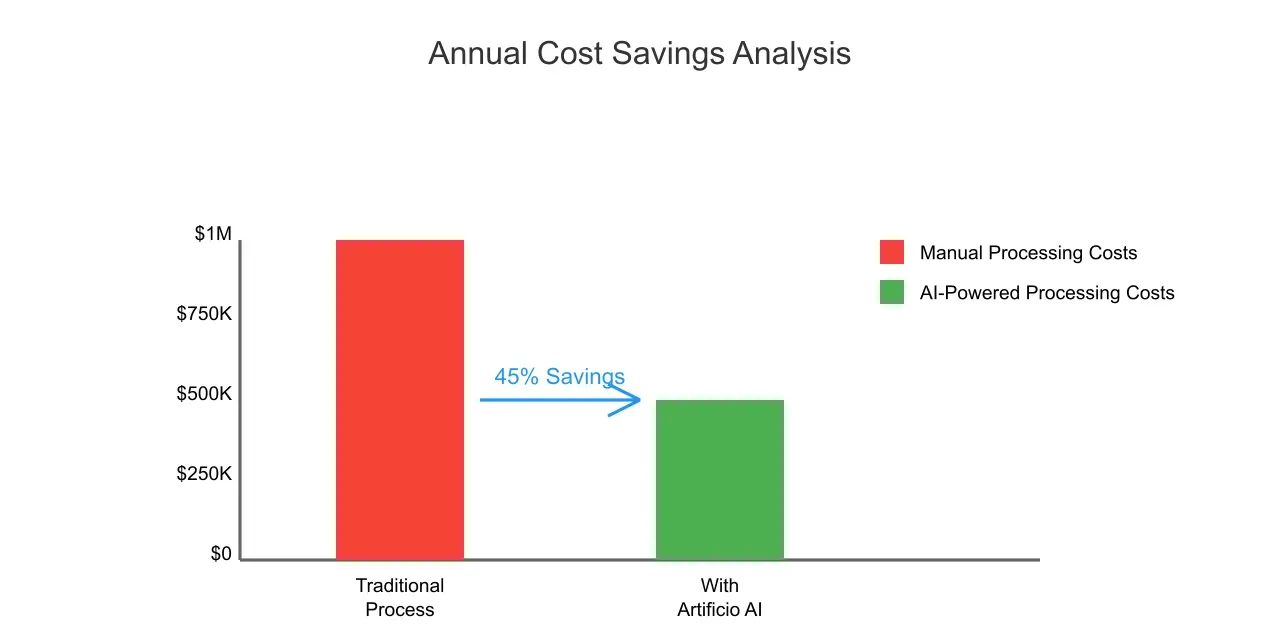
Cost Reduction: Implementation has led to an average 45% reduction in claims processing costs.
Revenue Cycle Improvement: Organizations report 15-20% faster revenue cycle completion due to reduced processing delays and fewer errors.
Resource Optimization: Staff reallocation to higher-value tasks has resulted in improved operational efficiency and staff satisfaction.
 Quality and Compliance Improvements
Quality and Compliance Improvements
Error Reduction: Manual entry errors reduced by 91%, leading to fewer claim rejections and resubmissions.
Compliance Enhancement: Automated compliance checking has resulted in a 96% reduction in compliance-related claim rejections.
Documentation Accuracy: Improved documentation accuracy has led to a 78% reduction in requests for additional information from payers.
Case Studies
Large Hospital System Implementation
A 500-bed hospital system implemented Artificio's solution across their network:
Initial State:
Average processing time: 22 minutes per claim
Manual error rate: 8.5%
Staff dedicated to claims processing: 45 FTEs
Post-Implementation Results:
Average processing time: 4 minutes per claim
Error rate: 0.7%
Staff reallocation: 60% of claims processing staff reassigned to patient care support
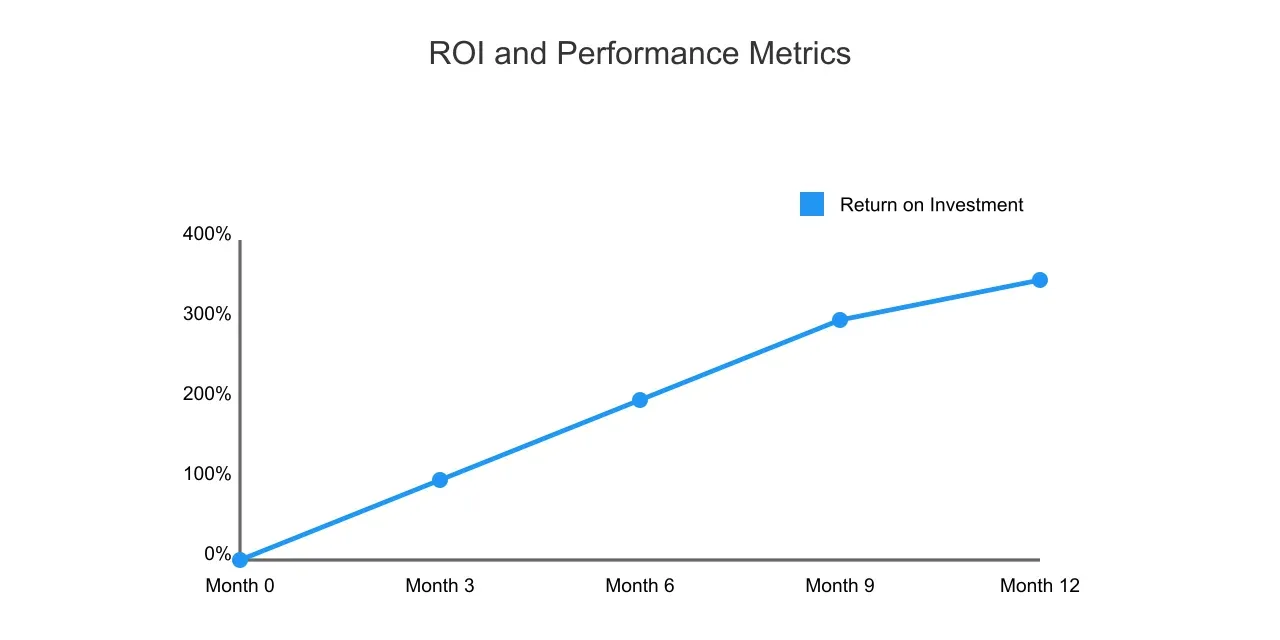
ROI achieved within 8 months
Multi-Specialty Clinic Network
A network of 12 specialty clinics implemented the system for outpatient claims:
Initial State:
Claims backlog: Average 12 days
First-pass resolution rate: 65%
Daily manual processing capacity: 500 claims
Post-Implementation Results:
Claims backlog: Reduced to 1.5 days
First-pass resolution rate: 94%
Daily processing capacity: 2,000+ claims
Patient satisfaction improvement: 35%
Future Outlook and Conclusions
Emerging Trends and Future Developments
The landscape of medical claims processing continues to evolve, with several emerging trends that will shape the future of AI-powered solutions:
Advanced Analytics Integration
The next generation of claims processing systems will incorporate more sophisticated analytics capabilities:
Predictive Analytics: Enhanced ability to predict claim outcomes and potential processing issues before they occur, allowing for preemptive problem resolution.
Real-time Analytics: Implementation of real-time processing analytics to provide immediate insights into claims status and potential issues.
Enhanced Interoperability
Future developments will focus on improved integration capabilities:
Standardized Data Exchange: Implementation of FHIR and other emerging healthcare data standards to facilitate seamless data exchange between systems.
Cross-platform Integration: Enhanced ability to integrate with various electronic health record systems and practice management platforms.
Artificial Intelligence Advancements
Continued evolution of AI capabilities will bring new opportunities:
Deep Learning Implementation: Integration of more sophisticated deep learning models for improved accuracy in complex claims processing scenarios.
Natural Language Understanding: Enhanced ability to process and understand unstructured medical documentation and clinical narratives.
Recommendations for Implementation
Organizations considering the implementation of AI-powered claims processing should consider the following recommendations:
Strategic Planning
Develop a comprehensive implementation strategy that includes:
Clear Objectives: Define specific, measurable goals for the implementation, including target processing times and error reduction rates.
Resource Allocation: Ensure adequate resources are allocated for implementation, including staff training and technical support.
Change Management: Develop a robust change management plan to address organizational and cultural impacts of implementation.
Technology Assessment
Conduct a thorough assessment of current technology infrastructure:
System Compatibility: Evaluate existing systems for compatibility with AI-powered solutions.
Data Quality: Assess current data quality and implement improvements where necessary.
Security Requirements: Ensure all security and compliance requirements are addressed in the implementation plan.
Conclusions
The implementation of Artificio's AI-powered claims processing system represents a transformative opportunity for healthcare organizations to significantly improve their claims processing efficiency and accuracy. The demonstrated results across various implementation scenarios show consistent improvements in key performance metrics:
Processing Efficiency: Dramatic reductions in processing time and resource requirements.
Error Reduction: Significant decreases in error rates and claim rejections.
Cost Savings: Substantial reductions in processing costs and improved revenue cycle performance.
The success of implementations across different healthcare settings demonstrates the adaptability and scalability of the solution. Organizations that have implemented the system have consistently achieved positive ROI within the first year of implementation, with many reporting continued improvements in performance metrics over time.
As healthcare organizations continue to face increasing pressure to improve efficiency while maintaining accuracy and compliance, AI-powered claims processing solutions like Artificio's platform will become increasingly essential tools for maintaining competitive advantage and operational excellence.
