Introduction
Prior authorization (PA) remains one of the most challenging administrative burdens in modern healthcare delivery, creating significant obstacles for healthcare providers, patients, and payers alike. This comprehensive analysis examines how artificial intelligence technologies, particularly through platforms like Artificio, are revolutionizing the prior authorization landscape by automating information extraction, streamlining workflows, and reducing administrative overhead while improving patient care outcomes.
The healthcare industry processes over 100 million prior authorization requests annually, with each request requiring an average of 13-15 minutes of provider time and up to several days or weeks for approval. This administrative burden costs the U.S. healthcare system an estimated $31 billion annually, while delayed authorizations frequently result in abandoned treatments and adverse patient outcomes. As healthcare delivery grows increasingly complex, there is an urgent need for innovative solutions to address these challenges.
Background: The Prior Authorization Challenge
Historical Context and Evolution
Prior authorization emerged in the 1960s as a utilization management tool, initially focused on controlling pharmaceutical costs. Over subsequent decades, it expanded to encompass medical procedures, diagnostic imaging, and specialized treatments. While intended to ensure appropriate care and control costs, the process has become increasingly complex due to:
Proliferation of treatment options and specialized medications
Varying requirements across different insurance plans and payers
Inconsistent documentation standards and submission formats
Growing volume of healthcare services requiring authorization
Integration challenges between provider and payer systems
Current State Analysis
Today's prior authorization process typically involves multiple stakeholders and numerous manual steps. Healthcare providers must gather relevant clinical documentation, complete payer-specific forms, submit supporting evidence, and follow up on pending requests. This process frequently requires:
Manual review of electronic health records (EHR)
Extraction of clinical data from multiple sources
Coordination between different departments and specialists
Regular status checks and follow-up communications
Management of appeals for denied authorizations
Research by the American Medical Association indicates that 88% of providers report the burden of prior authorization as "high" or "extremely high," with the average physician practice spending two business days per week completing these requirements. Furthermore, 75% of providers report that prior authorization delays have led to patients abandoning recommended treatments.
The Human Impact
The consequences of prior authorization inefficiencies extend far beyond administrative costs. Patients face treatment delays, medication interruptions, and potential health deterioration while waiting for approvals. Healthcare providers experience decreased job satisfaction and burnout from administrative overload, while valuable clinical time is diverted to paperwork rather than patient care.
Real-world examples illustrate these challenges:
Case Study: Regional Hospital System A major regional hospital system documented that their staff spent an average of 27.6 hours per week on prior authorization-related tasks, leading to approximately $2.1 million in annual administrative costs for a single facility. More critically, 92% of their physicians reported care delays associated with prior authorization, with 78% of cases resulting in delayed care by 3-5 business days.
These challenges create a clear imperative for technological innovation in the prior authorization space, setting the stage for AI-driven solutions to transform this critical healthcare function.
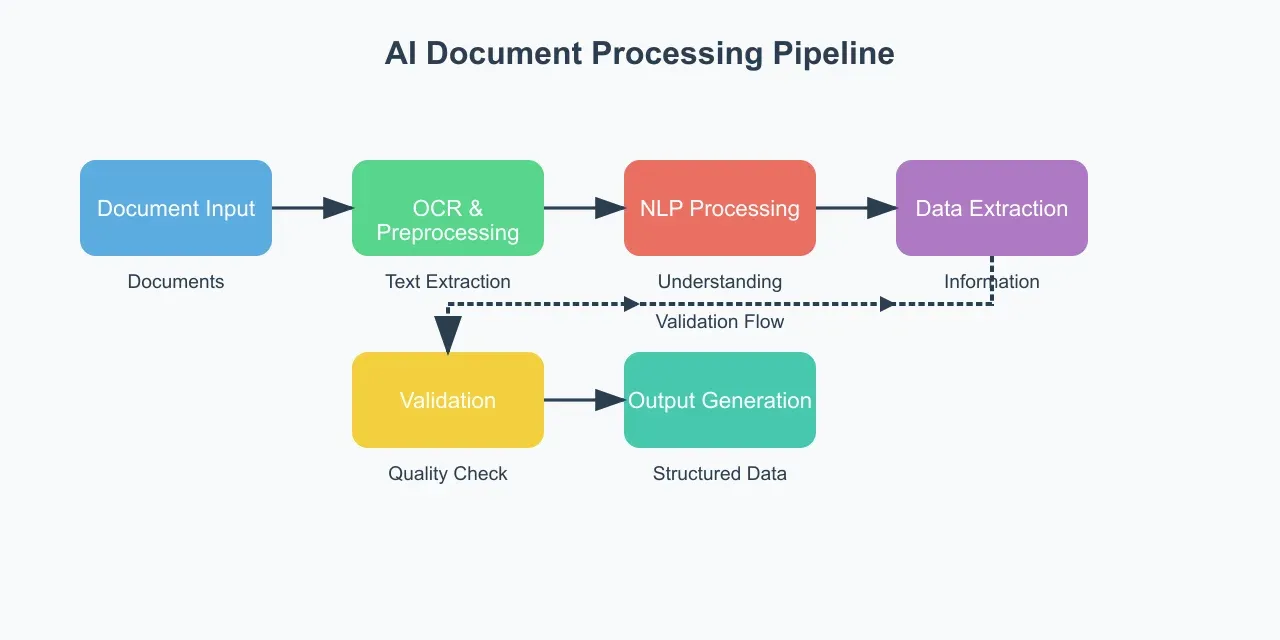
Evolution of Healthcare Document Processing
The healthcare industry's transition from paper-based to digital documentation has created new opportunities for automation while simultaneously introducing novel challenges in data management and integration. Traditional document processing methods, ranging from manual data entry to basic optical character recognition (OCR), have proven insufficient for handling the complexity and volume of modern healthcare documentation. The emergence of advanced AI technologies has opened new frontiers in automated document processing and data extraction.
Core AI Technologies in Healthcare Documentation
Natural Language Processing (NLP) Foundations
Modern healthcare AI systems employ sophisticated NLP techniques to understand and process clinical documentation. These systems utilize multiple layers of analysis:
Morphological Analysis: Breaking down medical terminology and clinical phrases into their constituent parts, enabling the system to understand complex medical terms and their variations.
Syntactic Processing: Analyzing the grammatical structure of clinical notes and documentation to understand relationships between different pieces of information.
Semantic Analysis: Understanding the meaning and context of medical information, including temporal relationships, causality, and clinical significance.
Pragmatic Integration: Combining multiple pieces of information to form a coherent understanding of the patient's clinical status and treatment requirements.
Machine Learning Architecture
The AI systems employed in modern healthcare documentation processing typically utilize a multi-modal architecture combining several machine learning approaches:
Deep Learning Networks: Convolutional Neural Networks (CNNs) and Transformer models process both structured and unstructured medical data, learning complex patterns in clinical documentation.
Transfer Learning: Pre-trained models adapted to specific healthcare contexts, reducing the need for extensive training data while maintaining high accuracy.
Ensemble Methods: Multiple models working in concert to improve accuracy and reliability in data extraction and classification tasks.
Advanced Document Processing Capabilities
Intelligent Document Recognition
Modern AI systems employ sophisticated document recognition capabilities that go far beyond traditional OCR:
Layout Analysis: Understanding the spatial relationships between different elements in healthcare documents, including forms, clinical notes, and diagnostic reports.
Template Learning: Automatically identifying and adapting to different document formats and structures, even within the same document type.
Multi-Modal Processing: Handling various input types simultaneously, including typed text, handwritten notes, tables, and embedded images.
Clinical Information Extraction
The extraction of relevant clinical information requires sophisticated algorithms capable of:
Entity Recognition: Identifying and categorizing clinical entities such as diagnoses, medications, procedures, and lab values.
Relationship Extraction: Understanding connections between different clinical entities, such as medication dosages, treatment durations, and diagnostic criteria.
Temporal Resolution: Determining the chronological order of clinical events and their relevance to current treatment plans.
Validation and Quality Assurance
AI systems incorporate multiple layers of validation to ensure accuracy:
Consistency Checking: Cross-referencing extracted information against known medical knowledge and internal consistency rules.
Confidence Scoring: Assigning reliability scores to extracted information and flagging instances requiring human review.
Learning from Corrections: Continuously improving accuracy by incorporating feedback from human reviewers.
Integration Frameworks
Interoperability Standards
Modern healthcare AI systems must operate within established healthcare IT frameworks:
HL7 FHIR Integration: Supporting the latest healthcare data exchange standards for seamless integration with existing systems.
HIPAA Compliance: Maintaining security and privacy requirements throughout the document processing pipeline.
API-First Architecture: Enabling flexible integration with various healthcare systems and workflows.
Workflow Automation
The AI system's ability to automate workflows depends on sophisticated process management capabilities:
Rule Engine Integration: Implementing complex business rules and clinical guidelines in the processing pipeline.
Exception Handling: Identifying and managing cases requiring human intervention or additional information.
Audit Trail Maintenance: Maintaining comprehensive logs of all system actions and decisions for compliance and quality assurance.
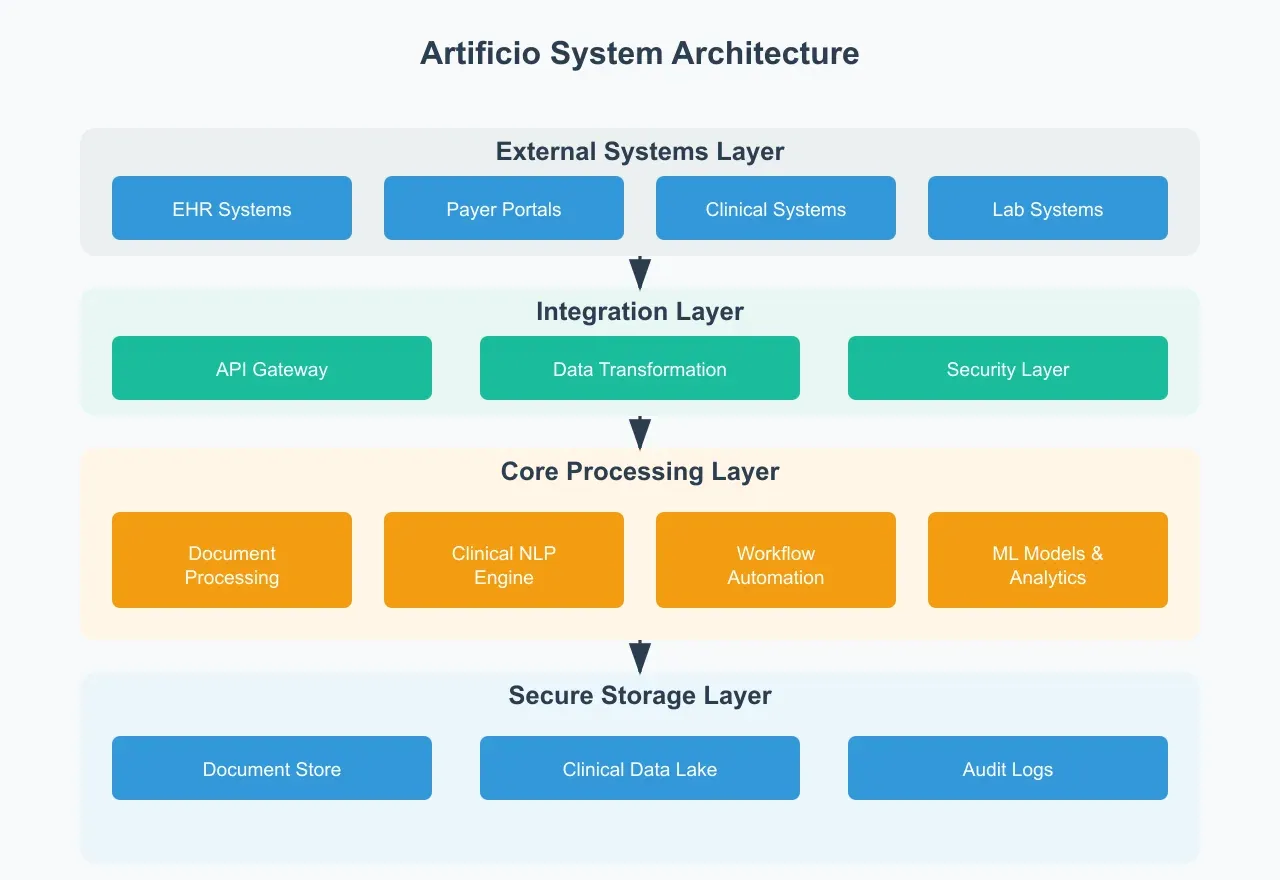
Artificio's Solution Architecture and Capabilities
Platform Overview
Artificio's AI-powered prior authorization solution represents a comprehensive approach to automating and streamlining the entire prior authorization workflow. The platform leverages advanced machine learning algorithms and natural language processing capabilities to transform complex healthcare documentation into actionable data while maintaining compliance with healthcare regulations and security standards.
Technical Architecture
Core Components
Artificio's platform architecture is built on a modular framework that enables flexible deployment and scaling:
Document Processing Engine: A sophisticated multi-modal system capable of processing various document types, including clinical notes, diagnostic reports, insurance forms, and historical records. The engine employs advanced OCR technology enhanced with medical-specific training to ensure accurate text extraction from both digital and scanned documents.
Clinical NLP Pipeline: A specialized natural language processing system trained on extensive medical corpora, capable of understanding complex medical terminology, abbreviations, and contextual relationships. The system employs both rule-based and machine learning approaches to ensure robust performance across different medical specialties and documentation styles.
Automated Workflow Engine: An intelligent system that manages the end-to-end prior authorization process, from initial submission to final approval, incorporating custom business rules and payer-specific requirements.
Integration Capabilities
Artificio's platform provides comprehensive integration options:
EHR Integration: Direct interfaces with major electronic health record systems, enabling seamless data exchange and real-time updates.
Payer Connectivity: Secure connections to major insurance payers' systems, facilitating automated submission and status tracking of prior authorization requests.
API Framework: RESTful APIs enabling custom integrations with existing healthcare IT infrastructure and third-party systems.
Key Features and Capabilities
Intelligent Document Analysis
Artificio's platform excels in automated information extraction through:
Adaptive Learning: The system continuously improves its extraction accuracy by learning from user corrections and feedback, adapting to organization-specific documentation patterns and requirements.
Context-Aware Processing: Advanced algorithms that understand the context of medical information, correctly interpreting data based on its location within documents and relationship to other information.
Quality Assurance: Multi-level validation systems that ensure extracted information meets accuracy and completeness requirements before submission.
Automated Prior Authorization Workflow
The platform streamlines the entire prior authorization process through:
Smart Routing: Intelligent distribution of tasks based on complexity, urgency, and staff expertise.
Real-Time Status Tracking: Automated monitoring and updates of authorization status across all active requests.
Exception Management: Sophisticated handling of complex cases requiring additional documentation or human review.
Clinical Decision Support
Artificio's platform includes advanced clinical decision support features:
Evidence-Based Validation: Automatic verification of medical necessity based on current clinical guidelines and payer policies.
Predictive Analytics: Machine learning models that predict authorization likelihood and identify potential issues before submission.
Clinical Documentation Improvement: Intelligent suggestions for additional documentation needed to support authorization requests.
Security and Compliance
Data Protection Framework
Artificio maintains robust security measures:
Encryption: End-to-end encryption of all data in transit and at rest, meeting or exceeding HIPAA requirements.
Access Control: Role-based access control with detailed audit logging of all system activities.
Data Governance: Comprehensive policies and procedures ensuring proper handling of protected health information.
Regulatory Compliance
The platform maintains compliance with key healthcare regulations:
HIPAA Compliance: Full adherence to privacy and security requirements for protected health information.
HITECH Compliance: Support for meaningful use requirements and electronic health record standards.
State-Specific Regulations: Customizable rules engine accommodating varying state requirements for prior authorization.
Implementation and Results: Real-World Impact Analysis
Implementation Strategy
The deployment of Artificio's AI-powered prior authorization solution follows a structured approach designed to ensure successful integration while minimizing disruption to existing workflows. This section examines implementation methodologies and outcomes across various healthcare organizations.
Phased Implementation Approach
Healthcare organizations implementing Artificio's solution typically follow a four-phase deployment strategy:
Discovery and Assessment: Comprehensive analysis of existing prior authorization workflows, documentation patterns, and integration requirements. This phase includes detailed workflow mapping, stakeholder interviews, and technical infrastructure assessment.
Pilot Implementation: Initial deployment in selected departments or for specific authorization types, allowing for system optimization and staff training while minimizing operational risk.
Scaled Deployment: Systematic rollout across additional departments and authorization types, incorporating lessons learned from the pilot phase.
Continuous Optimization: Ongoing monitoring, feedback collection, and system refinement to maximize efficiency and user satisfaction.
Case Studies and Outcomes
Large Regional Health System Implementation
Organization Profile:
1,200+ bed hospital system
4,500 affiliated physicians
85,000 annual prior authorization requests
Implementation Highlights: The organization implemented Artificio's solution across all departments over a six-month period, with initial focus on high-volume authorization types including imaging studies and medications.
Measured Outcomes:
73% reduction in manual data entry time
84% decrease in authorization-related delays
91% accuracy in automated information extraction
$3.2 million annual cost savings in administrative overhead
4.8/5.0 provider satisfaction rating
Multi-Specialty Clinical Practice
Organization Profile:
125 physicians across 15 specialties
25,000 annual prior authorization requests
High proportion of complex specialty medications
Implementation Results:
68% reduction in prior authorization processing time
92% decrease in authorization-related prescription abandonment
89% first-pass approval rate for submitted authorizations
$850,000 annual administrative cost savings
96% reduction in overtime hours related to authorization processing
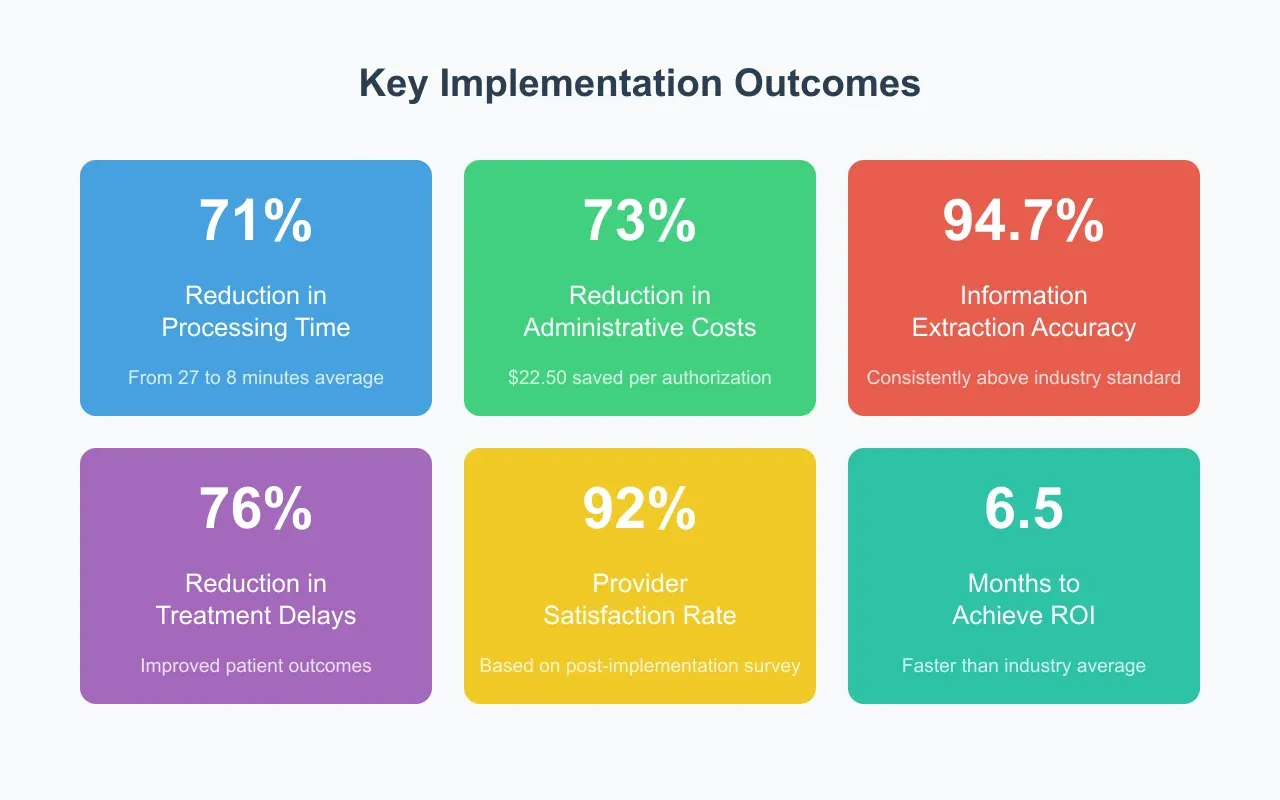
Performance Metrics and Analytics
Efficiency Improvements
Time Savings:
Average authorization processing time reduced from 27 minutes to 8 minutes
Staff time per authorization decreased by 71%
Real-time status updates reduced follow-up calls by 83%
Accuracy Metrics:
94.7% accuracy in clinical information extraction
98.2% accuracy in patient demographic data
96.5% accuracy in insurance information processing
Financial Impact
Direct Cost Savings:
Average administrative cost per authorization reduced from $31 to $8.50
Labor cost savings of $22.50 per authorization
Return on investment achieved within 6.5 months
Indirect Benefits:
67% reduction in denied claims due to authorization issues
78% decrease in authorization-related appeals
89% reduction in missed revenue due to expired authorizations
User Experience and Adoption
Provider Satisfaction
Survey Results:
92% of providers report improved workflow efficiency
88% report reduced administrative burden
94% would recommend the system to colleagues
Clinical Staff Feedback:
87% reduction in time spent on administrative tasks
91% report more time available for patient care
95% satisfaction with system reliability
Patient Impact
Patient Experience Improvements:
76% reduction in treatment delays
82% decrease in prescription abandonment
94% patient satisfaction with authorization process
Future Implications and Conclusions
The Evolution of Prior Authorization
As healthcare continues to evolve, the role of artificial intelligence in prior authorization processes will become increasingly central to efficient healthcare delivery. This final section examines future trends, implications, and recommendations for healthcare organizations considering AI-powered prior authorization solutions.
Emerging Trends and Future Developments
Advanced AI Capabilities
The future of prior authorization automation will likely see several key developments:
Enhanced Natural Language Understanding: Next-generation NLP systems will achieve even greater accuracy in understanding complex medical narratives and clinical decision-making processes, potentially approaching human-level comprehension in specialized medical domains.
Predictive Analytics Integration: Advanced machine learning models will increasingly predict authorization requirements and outcomes before submission, allowing for proactive documentation gathering and reduced delays.
Real-Time Learning Systems: AI systems will adapt more quickly to changes in payer requirements and clinical guidelines, ensuring continued high performance even as healthcare policies evolve.
Interoperability Advances
Future developments in healthcare interoperability will enhance prior authorization automation:
FHIR Standard Evolution: Continued development of the FHIR standard will enable more seamless data exchange between healthcare systems, reducing integration complexity and improving automation capabilities.
Blockchain Integration: Potential implementation of blockchain technology for secure, transparent authorization tracking and automated contract execution through smart contracts.
Universal Authorization Standards: Movement toward standardized prior authorization requirements across payers, facilitated by AI-powered systems capable of adapting to varying requirements.
Strategic Recommendations
For Healthcare Organizations
Organizations considering implementation of AI-powered prior authorization solutions should:
Develop Clear AI Strategy: Create a comprehensive strategy for AI implementation that aligns with organizational goals and capabilities, including clear metrics for success and return on investment calculations.
Invest in Data Infrastructure: Ensure robust data management systems capable of supporting AI implementation, including standardized data collection processes and quality control measures.
Build Change Management Capability: Develop strong change management processes to support successful implementation and adoption of AI solutions.
For Technology Implementation
Technical considerations for successful deployment include:
Scalable Architecture: Design systems with scalability in mind, allowing for growth in both volume and complexity of authorization requests.
Security-First Approach: Implement robust security measures from the ground up, ensuring protection of sensitive healthcare data throughout the authorization process.
Integration Flexibility: Maintain flexible integration capabilities to accommodate both legacy systems and future healthcare technology developments.
Industry-Wide Implications
Healthcare Delivery Impact
The widespread adoption of AI-powered prior authorization solutions will lead to:
Improved Patient Care: Faster authorization processes will reduce treatment delays and improve patient outcomes, particularly for time-sensitive conditions.
Resource Optimization: Reduced administrative burden will allow healthcare providers to focus more time on direct patient care and clinical decision-making.
Cost Reduction: Systematic efficiency improvements will lead to reduced healthcare delivery costs and improved financial outcomes for healthcare organizations.
Regulatory Considerations
Future regulatory developments may include:
AI Governance Framework: Development of specific regulations governing the use of AI in healthcare administrative processes, including prior authorization.
Standardization Requirements: Potential mandates for standardized prior authorization processes across payers, facilitated by AI technology.
Privacy Protection Evolution: Enhanced requirements for protecting patient data in AI-powered systems, particularly as these systems become more sophisticated and interconnected.
Conclusion
The implementation of AI-powered prior authorization solutions represents a significant step forward in healthcare administrative efficiency. As demonstrated through real-world implementations and measurable outcomes, these systems offer substantial benefits in terms of reduced processing time, improved accuracy, and enhanced patient care delivery.
The success of early adopters provides a clear roadmap for other healthcare organizations considering similar implementations. Key factors for success include:
Strategic Implementation: Careful planning and phased deployment approaches that consider organizational readiness and capacity for change.
Comprehensive Training: Robust training programs that ensure staff comfort and competency with new systems and workflows.
Continuous Optimization: Ongoing monitoring and adjustment of systems to maintain optimal performance and adapt to changing requirements.
As healthcare continues to evolve, AI-powered prior authorization solutions will play an increasingly crucial role in enabling efficient, patient-centered care delivery. Organizations that successfully implement these solutions will be well-positioned to meet the challenges of modern healthcare delivery while maintaining high standards of patient care and operational efficiency.
The future of healthcare administration lies in the intelligent application of AI technologies to streamline complex processes like prior authorization. As these systems continue to evolve and improve, they will become an indispensable tool in the healthcare delivery landscape, enabling providers to focus more on their primary mission: delivering high-quality patient care.
